Final assessment-Long case
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
A 60year old male patient presented to the OPD complaining of loss of consciousness since 4days and one episode of vomiting the next day
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 12 years back.
He then developed diabetes for which he is taking medication since 12years
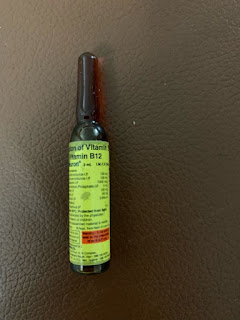
He used to take a regular dose of insulin IV and Glimepiride to control the sugar levels
One year back patient had burnt injury due bike silencer for which he did not take proper medication.Later the injury got infected and developed non healing ulcer which finally led to amputation of his three toe fingers 4months back.
After the surgery he stopped taking insulin IV and started taking Glimepiride bd
5Days back he attended a function where he took 90ml of alcohol and also he skipped his medication on that particular day.
On that particular day he fell unconscious due uncontrolled sugar levels and had one episode of vomiting the next morning.Vomiting -food as particles,non-projectile and non-bilious in nature
HISTORY OF PAST ILLNESS
Known case of DM since 12years
He underwent amputation 4months back
Patient has habit of consuming alcohol since 15years
Initially he used to consume alcohol daily -180ml
After the surgery he started consuming occasionally
No history of hypertension,asthma,TB,epilepsy
PERSONAL HISTORY
FAMILY HISTORY
History of diabetes was also found in patients siblings













Comments
Post a Comment